Team Tony cultivates, curates and shares Tony Robbins’ stories and core principles, to help others achieve an extraordinary life.
The health coach revolution
To change behaviors that lead to chronic disease, doctors aren’t enough
This article was contributed by special guest Chris Kresser – see full bio below.
Did you make a New Year’s resolution this year? How did it turn out?
If you’re like most people, you didn’t get very far. In fact, a commonly cited statistic suggests that only 8% of people keep their resolutions. That means that 92% of people fail!
There are many reasons for this, but they can be summed up this way: Changing our behavior is hard, and most people don’t know how to do it successfully. As far as resolutions go, many people choose to focus on their health during the new year. They want to lose weight, be more active for their family or just feel more energy. Despite these important reasons for wanting to get healthy, the majority of people still fail.
This is a huge problem, because it is now clear that the number one cause of the chronic disease epidemic is not genetic, but behavioral – people making the wrong choices about diet, physical activity, sleep and other lifestyle factors that ultimately impact their health.
In fact, a recent study found that 85% of the risk of chronic disease is due to these environmental factors. Another study found that fewer than 5% of adults engage in the top health behaviors, and only 20% of adults are thriving.
The consequences of neglecting our health are severe:
- One in two Americans has a chronic disease; one in four has multiple chronic diseases.
- Seven of ten deaths in the United States are caused by chronic disease.
- 27% of children now have a chronic disease (up from 13% in 1994).
- Chronic disease will account for $47 trillion in healthcare expenditure by 2030 if the epidemic is unchecked. That’s more than the annual GDP of the six largest economies in the world.
Given these statistics, it should be clear that 1) chronic disease is the biggest threat to our health that we face, and 2) changing our behavior is the most important step we can take to prevent and reverse chronic disease.
We don’t need more information – or more doctors – to solve this problem
It’s tempting to think that we can solve this problem simply by better educating people about the health changes they need to make. But it is now well established that knowledge is not enough to support lasting behavioral changes. Think about it: How many health-related PSAs have you seen in your lifetime? This type of informational briefing is not enough to better the health of the nation. If it was, we wouldn’t have divorced marriage counselors, crazy shrinks or doctors that smoke cigarettes!
Most people know that eating poorly, not exercising, not getting enough sleep and engaging in other unhealthy lifestyle habits is not good for them. Yet they continue these behaviors anyway, or they chase quick fixes that don’t last for more than a few weeks, such as briefly following intense New Year’s resolutions surrounding crash diets and extreme exercise regimes.
What about doctors? Shouldn’t they be the ones to lead this change? We simply don’t have enough of them to address the problem. The most recent statistics suggest that we’ll have a shortage of 52,000 primary care physicians by the year 2025.
But even if we didn’t have a shortage of doctors, most of them have neither the training nor the time necessary to support people in making lasting behavioral changes. The same is true for most other healthcare professionals, including nurse practitioners and physician assistants.
We could start training doctors and other healthcare providers in this area, but that still wouldn’t solve the problem. Our “sickcare” system is not set up to deliver this type of care. The average visit with a primary care provider in the United States is ten to twelve minutes, with newer doctors spending as little as eight minutes per visit with patients. That’s barely enough time to say hello, review the patient’s current medications, and possibly prescribe a new one. It’s not even remotely enough time to assess what behavior and lifestyle changes would be most effective for the patient and provide the support necessary for sustaining them for a lifetime, not to mention that healthcare can be so expensive that many people avoid going to the doctor altogether.
What’s more, doctors are trained in the “expert” approach of simply telling people what to do and expecting them to do it. That might work well when someone is facing a serious, acute health crisis (like appendicitis), but it fails miserably when it comes to long-term behavior changes like losing weight, managing stress or adopting a sustainable exercise routine. Doctors aren’t trained to work collaboratively with their patients. This is painfully reflected by the fact that patients get to speak for only 12 seconds on average before being interrupted with advice from their physician.
Health coaches are the solution
If more information and more doctors won’t solve the problem, what will?
Health coaches.
People want to feel good, avoid chronic disease and live a long life. They want to see their children and grandchildren grow up and have the energy to play with them. They want to perform better at work, enjoy their relationships, and be well enough to get the most out of life. But there’s a big difference between wanting the benefits of being healthy and consistently engaging in the behaviors that lead to health.
That’s where health coaches come in. What is a health coach? Health coaches are trained in a number of disciplines that support people in making lasting change. These include (but aren’t limited to):
- Positive psychology, which leverages people’s strengths (rather than focusing on their weaknesses) to make changes
- Motivational interviewing, which helps people to link behavior changes to their deepest needs and goals (e.g., “I will change my diet because I want to live to see my grandchildren graduate from college.”)
- Habit formation and reversal, which supports patients in making positive habits, or breaking negative ones
Coaches are also trained to work with patients in a more collaborative way, rather than with the expert approach that is common in medicine. In the expert approach, the “authority” assesses the problem, delivers advice, recommends solutions, and in some cases, teaches new skills. In the collaborative approach, the health coach acts as a partner or ally, encourages clients to discover their own solutions and become their own advocate and supports them in developing the skills they need to embrace new behaviors.
This collaborative approach empowers the client to become the primary driver of change. That’s why you need a health coach – it also builds confidence, self-awareness and self-actuation – all of which are crucial for long-term change, since the client will likely not work with the coach for the duration of his or her lifetime. To use the old analogy, the doctor gives the patient a fish so she can eat for a day, whereas the coach teaches the client to fish so she can eat for a lifetime.
Not surprisingly, studies have consistently shown that coaching interventions improve health outcomes for several chronic diseases, including diabetes, heart disease, obesity, and cancer. This is not a small effect. In fact, some research has shown that applying evidence-based principles of behavior change can increase the chances of success by over 1,000%!
A visit with a health coach is often more affordable than a visit with a doctor, whether the client is paying directly or the insurance company is covering it. This is critical, because more frequent visits are required to support effective behavioral change.
Along the same lines, the barriers to entry to become a health coach are significantly lower than to become a doctor, nurse practitioner, or physician assistant. This is also important, because we’ll need at least ten times the number of health coaches than doctors in order to make a significant dent in preventing and reversing chronic disease.
Coaches and doctors working together: the best of all worlds
By no means should you stop seeing a doctor entirely. Doctors and other licensed clinicians will always be required to order lab tests, analyze those results, diagnose disease, prescribe treatment and coordinate care. Health coaches aren’t trained to do those things, just as doctors aren’t trained to support behavioral changes. However, to not only remain in top physical health but to modify negative behaviors, you should see both a doctor and a health coach on a regular basis.
The strongest approach would be one that utilizes the professional that is best trained and suited for each particular need: Health coaches to support diet, lifestyle and behavior change and doctors to practice medicine.
What would this look like in practice? Imagine the healthcare population as a pyramid:
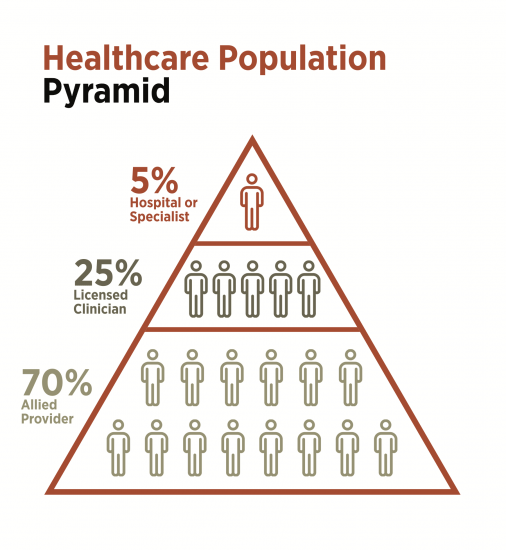
The top 5% of the pyramid – those experiencing acute or emergency problems that require intensive care, often in a hospital or specialized setting – are best served by conventional medical intervention.
The 25% of patients in the middle of the pyramid – those dealing with fairly significant chronic health challenges – will likely require the ongoing support of a licensed clinician (ideally practicing Functional Medicine) but would also benefit from working with a health coach to implement the recommendations of the licensed provider. By getting a doctor’s opinion and working with a knowledgeable health coach to execute healthier lifestyle choices, patients can actively manage chronic health conditions.
The 70% of patients at the bottom of the pyramid – those with less severe chronic health problems, or those who are generally healthy – might be best served by working primarily with a health coach, with occasional visits with a doctor for labs, check-ups, etc.
This approach would not only be more effective for preventing and reversing chronic disease, but it would also save us an enormous amount of money. Given that we spend nearly $4 trillion on healthcare each year, if utilizing health coaches could reduce that by even 25% (which is entirely reasonable) that would save us a trillion dollars a year. That’s no small thing, since some estimates suggest that the United States will be bankrupt by the year 2035 if healthcare spending continues to increase at its current pace. And since medical expenses are the number one cause of individual bankruptcy, using health coaches in this way could have a significant impact on each American’s pocketbook as well.
The writing is on the wall: chronic disease is destroying our quality of life, shortening our lifespan, bankrupting our country and threatening the health of future generations. It’s clearer than ever that our “disease management” system, which was designed to address medical emergencies and other acute conditions, is not prepared for the challenge of chronic disease or preventative care. We desperately need a new solution – one that is affordable, timely and suitable for the task at hand. In short, that’s why we need a health coach revolution!
About Chris Kresser
Chris Kresser is the author of Unconventional Medicine: Join the Revolution to Reinvent Healthcare, Reverse Chronic Disease, and Create a Practice You Love, a book for healthcare practitioners and the general public that proposes a bold solution to the chronic disease epidemic. He is also the founder of Kresser Institute, an organization that trains healthcare practitioners in applying Functional Medicine and an ancestral diet and lifestyle in their practices; the creator of ChrisKresser.com (one of the top natural health websites in the world); and the New York Times best-selling author of The Paleo Cure. His new book Unconventional Medicine will be released on November 7th.